Researchers at Columbia University Fertility Center have reported the first successful pregnancy using an AI-guided method they developed to recover sperm in men with azoospermia, a condition in which ejaculate contains little or no sperm.
The case, described in a research letter published in The Lancet, demonstrates the potential of the technology to help couples overcome male-factor infertility, which accounts for approximately 40 per cent of infertility cases. Of those, about 10-15 per cent of men with infertility have azoospermia.
“A semen sample can appear totally normal, but when you look under the microscope you discover just a sea of cellular debris, with no sperm visible,” said Zev Williams, Director of the Columbia University Fertility Center. “Many couples with male-factor infertility are told they have little chance of having a biological child.”
Surgically extracted sperm
Men with azoospermia may undergo a procedure to have sperm surgically extracted from the testes, but the procedure is often unsuccessful and can cause vascular problems, inflammation, or a temporary decrease in testosterone levels.
A few specialised labs employ technicians to manually inspect semen samples—a lengthy and expensive process — after they have been processed with a centrifuge or other agents that can damage sperm.
“The field has really been challenged to find a better way to identify and retrieve viable sperm cells in men with exceedingly low sperm counts,” said Williams.
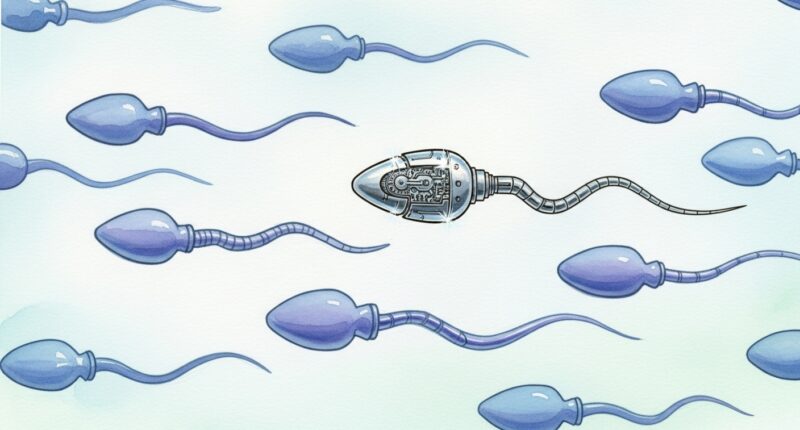
The STAR (Sperm Tracking and Recovery) method, unveiled earlier this year, employs high-powered imaging technology to scan through a semen sample from men with azoospermia, taking over 8eight million images in under an hour.
Artificial intelligence identifies sperm cells in the sample, and a microfluidic chip with tiny, hair-like channels isolates the portion of the semen sample containing the sperm cell. Within milliseconds, a robot gently removes the sperm cell so that it can be used to create an embryo or frozen and stored for future use.
“Our team included experts in advanced imaging techniques, microfluidics, and reproductive endocrinology to tackle each individual step required to find and isolate rare sperm,” said Hemant Suryawanshi, assistant professor of reproductive sciences at Columbia University Vagelos College of Physicians and Surgeons and project leader.
STAR was tested in a patient who had been trying to start a family for nearly 20 years, including multiple IVF cycles at other centres, several manual sperm searches, and two surgical procedures to extract sperm. The patient provided a 3.5 ml semen sample. In about two hours, STAR scanned 2.5 million images, identifying two viable sperm cells, which were then used to create two embryos and start a pregnancy.
“You only need one healthy sperm to create an embryo,” said Williams.
Larger clinical studies are underway to evaluate the efficacy of STAR in broader patient populations.